North Carolina health experts talk about ways to improve rural medicine across the state
This past Tuesday, the North Carolina Healthcare Association had rural health experts speak about how their hospitals and health systems in rural North Carolina are reimagining health care to ensure their communities have the resources they need close to home.
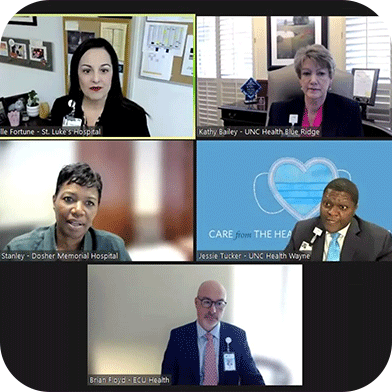
Executives and rural healthcare leaders from St. Luke’s Hospital, UNC Health Wayne, UNC Health Blue Ridge, Dosher Memorial Hospital, and ECU Health spoke on their efforts to improve access and care in rural communities with outside-of-the-box thinking and collaborative partnerships.
Brian Floyd of ECU Health noted that despite the Hill–Burton Act providing federal grants to states for the construction of new community hospitals that would be operated on a nonprofit basis, it was hard to realistically keep them open once those funds stopped and demand increased:
“They were never sustainable capital investments to begin with, without state and federal partnerships, to put those dollars in place to build those community hospitals. So we would be foolish to assume that they can just thrive in the absence of more invested interest of the local communities,” Floyd said.
Despite that difficult reality, experts also talked about ways to garner community support for local, rural hospitals.
Kathy Bailey of UNC Health Blue Ridge noted that hospitals are more than a physical lifeline for communities: “We are the economic pillars for so many of our communities where we’re the largest employer, usually.”
Experts discussed the need for community support — basically, trusting a local rural hospital and using its resources instead of traveling to larger hospitals in metro areas.
Longer term, experts talked about establishing a pipeline — getting rural children interested in healthcare at an early age, and training medical residents at rural hospitals — all with the hope they’ll pursue working in rural healthcare.
“Because we have to grow our own for those rural communities, not just a big pool of people that can go anywhere in the nation. We need the people in those communities to want to be in those communities and serve those communities through their local hospitals. Nothing works better. Trying to move people from urban environments into those rural environments can be very challenging. But the student that grows up in that community is the best, most likely candidate to help fill those gaps in the future,” Floyd said.
The introduction of Telehealth services has been a game-changer for accessibility, Bailey noted that their hospital set up a “virtual hospital” during the COVID-19 pandemic from 2020-2022, and successfully served over 12,000 patients. However, experts still noted that not everyone has access to reliable technology nearby.
Experts also discussed mobile health clinics and services, especially those that provide care to the under- and uninsured, as a way to make sure communities don’t feel forgotten.
The bottom line? Rural hospitals need outside financial investment, and internal community investment through engagement and job opportunities. Future healthcare workers have to see and commit to the vision of rural care, and be willing to work in those hard-to-reach places.